As Frost had pointed out in his oft quoted poem, traversing the road not taken makes all the difference in the world. As we live in these times of a pandemic, every day there is a barrage of information regarding the COVID-19 crisis. This ranges from the diagnostic information to the pathogenesis, infectivity, and spread of the virus. As clinicians, this information benefits us as much as the information about the precautions to be taken against the disease. One positive point is that the disease is preventable if we take precautions and that though it cannot cured, it can be recovered from. With the information that have been entrusted with, we have been pushed in the direction of searching for the new normal, to carve a road for the future of our practice.
What we started out with
The first clinical case regarding the COVID-19 virus was reported in Wuhan, China towards the tail end of December 2019. It was described as a strain of the Influenza virus that was more contagious than the ones previously encountered, debilitating the respiratory system in the affected people more than any other strain of the virus known to man. The symptoms reported by the patients includes Insomnia, dysgeusia, pyrexia, accompanied by cough. Since the symptoms experienced by the patients were not noticeable at first, many cases went undetected. This coupled with the recovery rate from the disease, standing at a good 55% at present caused many to dismiss the threat that it posed.
Ignorance is bliss seemed to be the motto of most of the political leaderships so the reactions ranged from trying to suppress reporting of the cases, to hoping for nature to take its course, expecting that the virus would just end up being a bout of seasonal flu. There were also some absurd claims about meat-eaters being more affected and innovative medicines to cure the disease but like all medical conditions, these claims ran their course by the month of May, wherein the World Health Organisation concluded its report by informing that the Coronavirus was here to stay. With this began the phase of coping with this crisis. World leaders came to a common conclusion that they have to allow people to work and live their lives albeit with some precautions in place.
What did we do
The medical fraternity stepped up in these dire times. The profession has been working tirelessly on many fronts to tackle the problem. They have been many on active duty at the hospitals taking care of the patients of this disease and those with co-morbid conditions since the coronavirus has a more severe impact on immunocompromised patients. The clinicians are also working simultaneously to publish articles of their observations in patients to disseminate information amongst the community and the general public for diagnosis. Medical equipment suppliers have been designing personal protective equipment to prevent the spread of the disease amongst workers.
In the report of the U.S Department of Labour published by the World economic forum, the Dentists are at high risk of being infected by the virus. Since our profession involves a close contact with the patient while working in the Oral cavity which is the principal disseminator of the virus, the profession had been up in arms at the start of the pandemic, but it has been actively adapting. The professionals deferred elective dental procedures, adopted tele-consulting, performed emergency dental procedures while wearing PPE kits.
Begin again
A survey done by Brazilian clinicians during this time showed that Orthodontic patients were more apprehensive about their treatment being delayed than getting infected by the Coronavirus. Keeping this is mind the Orthodontic clinics are opening up again with revised standard operating procedures for the benefit of the clinician and the patient. These can be broadly categorised as
Preparatory Phase
1. Impetus on crowd management-As clinicians(especially as Residents) we are often time bound by appointments and yet attempt to cater to as many patients as one can, this trend must change. Patients too have to be made to understand the importance of reporting to the clinic for their scheduled appointments to prevent the close contact with a crowd of unknown patients. Tele-dentistry is encouraged now.
2. Use of physical barriers in the form of peri-glass or plastic partition in between working chairs
3. Use of HEPA filters -The COVID-19 virions are spherical particles with diameters of approximately 0.125 microns. The smallest particles are 0.06 microns, and the largest is 0.14 microns.
HEPA filters can filter out over 99% of the coronavirus in a single pass(via diffusion). The filter designs are available which can installed in split a AC setup, helpful in reducing the inventory.
4. Ventilation in clinics has to be maintained by Air circulation in clinics. A closed environment are detrimental for aerosol management following the use of rotary instruments. This will have to be improved in clinics through a frequent opening of windows or using an independent exhaust blower. Ceilings fans should be avoided. In centrally air-conditioned set-ups: blocking off the return air vents in the patient area to temporarily stop air circulation.
5. Display visual alerts at the entrance of the facility and in strategic areas (e.g., waiting for areas or elevators) about respiratory hygiene, cough etiquette, social distancing, and disposal of contaminated items in trash cans will have to be placed.
6. Installation of glass or plastic barrier at the reception desk, preferably with a two-way speaker system.
7. Distant waiting chairs, preferably a meter apart.
8. All areas to be free of all fomite such as magazines, toys, tv remotes or similar articles.
9. Cashless/contactless payment methods are preferred.
10. A bin with a lid should be available at triage where patients can discard used paper tissues.
11. Changing room to be available for staff and all workers to wear surgical top1and pyjama and clinic shoes
12. Dedicated area for donning and doffing of PPE.
13. Sensor taps or taps with elbow handles in the washrooms
14. The dental chair water lines should be equipped with ant retraction valves 15. Use of hand pieces with anti-retraction valves only
Implementation Phase
1. Since the infection spreads through close contact, diligent maintenance of patient records is needed now more than ever for contact tracing. Proper screening of the patient including detailed history taking. Temperature check (it does not test COVID but pyrexia) along with sanitisation procedure. Education about hygiene through posters at strategic points
2. We should educate patients that the should not carry any bags, or wear watches or other stuff which needs to be kept away during the procedure. Minimum contact of patient with the operatory.
3. Use of disposable chair covers and PPE including head cap, nitrile gloves, bouffant,3 ply masks, and face shields. Also, proper management of these disposables is of uttermost importance. As an alternative cotton chair covers, patient drapes and laminated surgical gown can also be encouraged as it can be autoclaved and reused. It is both cost effective and eco-friendly.
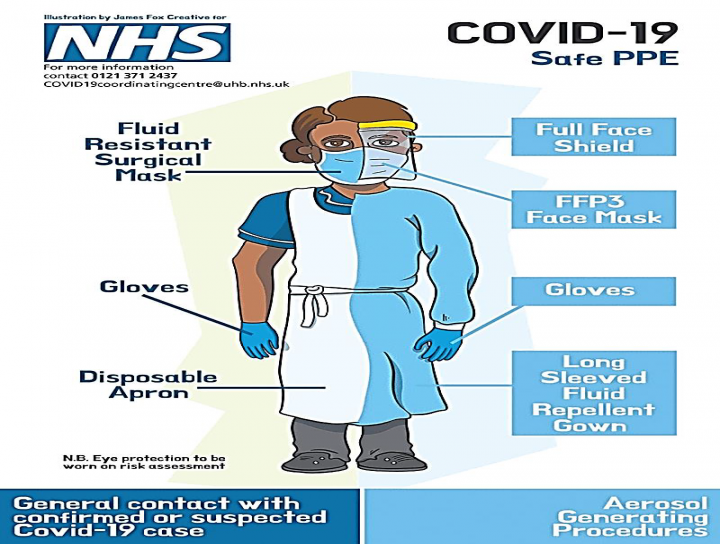
Personal protection equipment guidelines of the NHS-United Kingdom
4. Use of pre procedural mouth rinse
It has been investigated in vitro the viricidal effect of a mouthwash with PVP-I at 7%, diluted 1:30 in water, formulating a 0.23 % concentration, recommended for human use. It has been concluded that after 15 seconds of exposition, it succeeded in inactivating some pathogens like influenza virus A (H1N1), SARS-Cov, and MERS-Cov (Eggers et al., 2018).
Flowchart based on the American Dental Association Interim Guidance for Management of Emergency and Urgent Dental Care on 04/01/2020
What we should look forward to
With a host of research projects underway for finding a vaccine against and a cure for Covid-19 infections, now more than ever dental and medical fraternity is expected to educate themselves, keep abreast with the latest information and adopt the procedures being developed. These from the simplest procedures of automated sanitizer dispensers and advising patients over video calls, to learning sample collection methods from the infected patients.
Addressing the need for faster treatment outcomes of Orthodontic procedures and consequently lesser patient appointments, Accelerated Orthodontics will take precedence.
The Global economy has been negatively impacted by the pandemic hence many patients will be posed with a choice of continuing their Orthodontic treatment or deferring it for more pressing expenses. As an industry, Orthodontists must be receptive to this. The companies manufacturing the equipments used and materials developed must take cognizance of this and develop more economically viable alternatives for patients without compromising the quality of the treatment.
In conclusion, as Lord Tennyson wrote not once or twice in our rough island story, the path of duty is the path to glory’ so it shall be for Orthodontists as well. We should continue to serve our patients and our profession with renewed vigor.


No Any Replies to “Establishing the New Normal”
Leave a Reply