Organ transplantation is a life-saving procedure that requires careful preoperative assessment to minimize risks and ensure successful outcomes. One often-overlooked factor in transplantation is oral health. Oral infections, including periodontitis, dental abscesses, and untreated caries, can have a profound impact on transplant success by increasing the risk of systemic infections, graft rejection, and post-transplant complications.
Oral Infections as a Source of Systemic Complications
Oral infections harbor pathogenic bacteria that can enter the bloodstream, leading to bacteremia and systemic inflammation. In immunocompromised transplant recipients, such infections can have severe consequences, including:
Increased Risk of Sepsis: Oral bacteria, such as Streptococcus and Porphyromonas species, can contribute to systemic infections that may compromise transplant success.
Endocarditis: Dental infections can cause bacterial endocarditis, particularly in patients with pre-existing heart conditions or those receiving heart transplants.
Delayed Healing and Rejection: Chronic inflammation triggered by oral infections may contribute to transplant rejection by activating the immune response against the graft.
Pre-Transplant Dental Evaluation
To reduce the risks associated with oral infections, transplant candidates should undergo comprehensive dental evaluations before surgery. Key components of this assessment include:
Treatment of Active Infections: Extracting non-restorable teeth, treating periodontal disease, and addressing any existing abscesses.
Professional Cleaning and Oral Hygiene Education: Reducing bacterial load through scaling, root planing, and patient education on oral hygiene practices.
Collaboration Between Dentists and Transplant Teams: Ensuring that dental treatments are completed well in advance to allow adequate healing before immunosuppression therapy begins.
Post-Transplant Oral Health Considerations
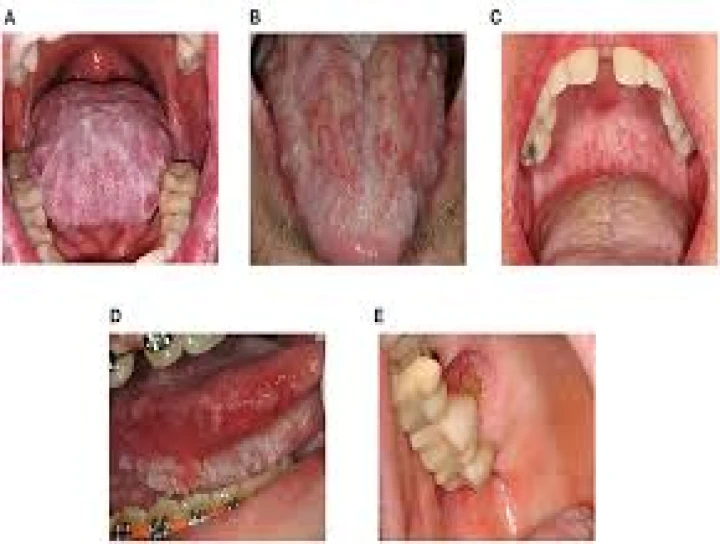
After transplantation, patients are placed on lifelong immunosuppressive therapy, increasing their susceptibility to infections. Common oral health concerns in post-transplant patients include:
Opportunistic Infections: Conditions like oral candidiasis and viral infections (e.g., herpes simplex) may arise due to immunosuppression.
Medication-Related Side Effects: Immunosuppressants such as cyclosporine can cause gingival overgrowth, necessitating careful oral hygiene and professional management.
Regular Dental Monitoring: Routine check-ups and preventive care are essential to promptly detect and manage oral health issues.
Conclusion
Oral infections pose a significant risk to organ transplant patients by increasing the likelihood of systemic infections, delayed healing, and graft rejection. Pre-transplant dental evaluations and post-transplant oral care are crucial in minimizing these risks. A multidisciplinary approach involving transplant specialists, dentists, and patients is essential to ensure optimal outcomes and long-term success of organ transplantation.


No Any Replies to “Impact of Oral Infection on Organ Transplantation”
Leave a Reply