Owing to its suburban location, the department receives a decent load of Oral Cancer patients. The department has optimum infrastructure with proficient maxillofacial surgeons to manage these patients with a holistic approach following effective protocols.
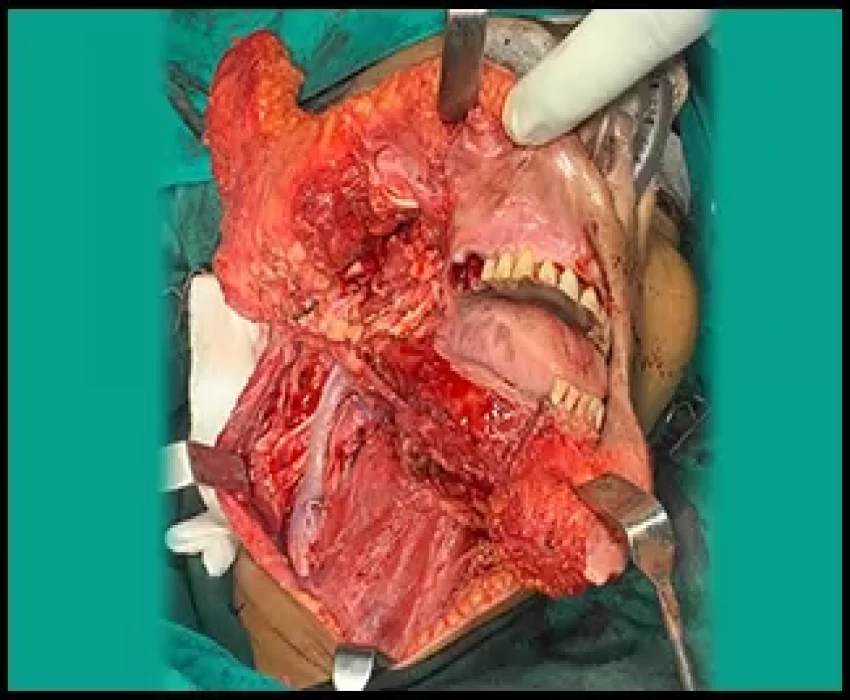
The Oral and Maxillofacial Surgery department of Saraswati Dental College and Hospital is fully equipped with ultramodern operation theatres, state of the art anesthesia machine and a backup of trained anesthetists and physicians to handle premalignant lesions, oral malignancies, benign and aggressive tumors of the facial region. The department follows an evidence-based approach towards the management of such conditions.Resection and radical neck dissection followed by various options for reconstruction has drawn the attention in today’s scenario where achieving the function with minimal morbidity is the key. The ladder for reconstruction has evolved over decades where local and regional flaps are now gradually getting replaced with free microvascular flaps. The rehabilitation using microvascular flaps that can incorporate both hard and soft tissue replacement with later incorporation of dental implants in the vascularized bone segments is the emerging trend in the field of maxillofacial surgery.
Surgical intervention allows the complete excision of a tumor and lymph nodes, followed by a full histologic examination for staging, which has implications for prognostication and assessing the need for adjuvant radiotherapy. Surgery can also be used for radioresistant tumors. Disadvantages are mainly the perioperative mortality and morbidity, but modern techniques have significantly decreased these adverse outcomes as well as decreased the aesthetic and functional defects that result from surgery.
Patients who succumb to oral cancer usually die because of failure to control the primary malignancy or because of nodal metastases. Death because of distant metastasis is unusual. Ablative surgery excises the cancer with, ideally, at least a 2-cm margin of clinically normal tissue. If a node has clinical signs of invasion, it is reasonable to assume that other nodes may also be involved, and they must be removed by traditional radical neck dissection. “Functional” neck dissections, modified to preserve the jugular, sternomastoid, or accessory nerve while ensuring complete removal of involved nodes, have gained popularity. Moderate-dose radiotherapy is sometimes used to “sterilize” cervical nodes affected by metastatic disease.
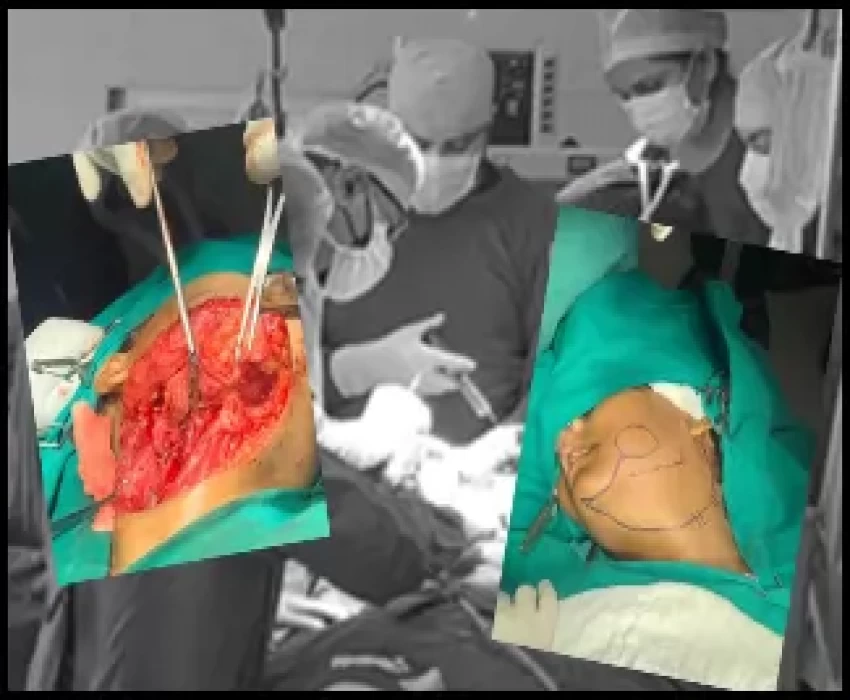
Reconstruction
Reconstruction is tailored to the patient's ability to cope with a long operation and the risk of substantial morbidity.
Soft-tissue reconstruction
Local flaps (such as nasolabial flaps) provide thin, reliable flaps suitable for repairing small defects. Often, however, tissue must be brought into the region to repair large defects. For these larger areas, split skin grafts or flaps—free or pedicle—are required.
Free flaps. Microvascular surgery facilitates excellent tissue reconstruction in a single operation by using free flaps. For example, forearm flaps based on radial vessels are particularly useful when replacing soft tissue. Flaps based on the fibula may be used if bone is also required.
Pedicle flaps. Myocutaneous or osteomyocutaneous flaps are based on a feeding vessel to muscle and perforators to the skin paddle. These flaps may be used in a 1-stage operation to replace skin, and because they also contain muscle, they have adequate bulk to help repair defects. Pedicle flaps may also be used to import bone (usually rib). Examples include flaps based on the pectoralis major, latissimus dorsi, or trapezius muscles. Flaps from the forehead or deltopectoral pedicle were once the mainstay for reconstruction, but they required a 2-stage operation, replaced only skin, and relied on a tenuous blood supply.
Hard-tissue reconstruction
Ideally, hard-tissue reconstruction is performed at the time of tumor resection. Dental implants can then be inserted to accommodate a dental prosthesis. Bone is traditionally in the form of free nonvascularized bone grafts taken from the iliac crest or a rib, but these grafts may survive poorly if contaminated or the vascularity is impaired after irradiation. In such cases, or when the defect is large, an osteomyocutaneous flap improves the graft's vascular bed. True free vascularized bone grafts such as fibula grafts have great benefits, but they are time-consuming to perform and require considerable expertise.
The benefits of bone grafting for maxillary defects are less certain, and maxillary reconstruction is usually accomplished with an obturator (bung), which has the advantage that the cavity can subsequently be inspected.
Surgical complications in patients with oral cancer may include infection, carotid artery rupture, salivary fistulae, and thoracic duct leakage (chylorrhea).